We are preparing for a new way of working in our practice. The idea is that we take what we do, and we supercharge it. Some of it sounds quite obvious.
Take the review of chronic diseases. At the moment, patients get called in for a pre-appointment check, then come back to see the nurse practitioner for a review of their condition.
The change is quite simple and also completely revolutionary. After the pre-appointment check, the patient is sent an update on their health, including any important areas to discuss, and space for them to consider what the key issues are for them. When they come to meet the nurse practitioner, the patient gets to choose which aspect of their health is most important for review, and for choosing which goals to set for the year ahead.
One of the key steps is how we reframe the review appointments. I personally believe that this is crucial: if we as a practice don’t understand and embrace this step, then all of the other changes are not going to be fully effective. This is the goal, the inspiring change.
I was very pleased to come across an article in the British Journal of General Practice: Setting goals with patients living with multimorbidity. Even the title is great – the goals are set with the patients, and they are the ones who are living with multimorbidity. The full article is in depth, and qualitative. The authors analyised 10 hours of VC to determine how goal setting is done. They describe ‘bearing witness’ to the patients goals. They conclude that this process requires a lot of time and energy from both parties, and it worked best when both GP and patient were prepared in advance.
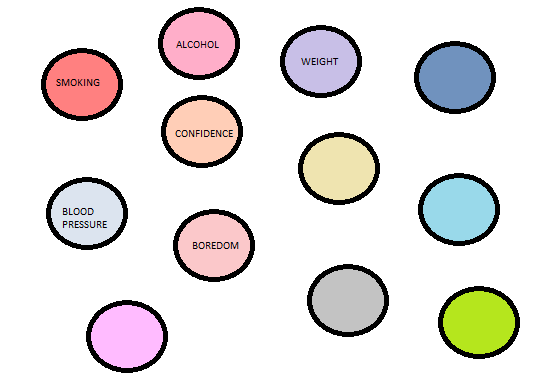
I’m keeping that summary in mind, both for when we attend our training in Harris, and for when I prepare the staff-room QI noticeboard.